Mortality Rates of Prostate Cancer
Welcome, reader! Let’s talk about the mortality rates of prostate cancer. Prostate cancer is one of the most common types of cancer among men, affecting thousands of individuals each year. Understanding the mortality rates associated with this disease is crucial for early detection and effective treatment. Join us as we delve into the statistics and research surrounding prostate cancer mortality rates, shedding light on this important health issue.
Understanding Prostate Cancer
Prostate cancer is a common form of cancer that affects the prostate gland, which is a small, walnut-shaped gland that produces seminal fluid. This type of cancer usually grows slowly and initially remains confined to the prostate gland, where it may not cause any serious harm. However, in some cases, prostate cancer can be aggressive and spread to other parts of the body, leading to serious complications and even death.
Prostate cancer typically occurs in older men, with the risk increasing with age. African-American men and those with a family history of prostate cancer are also at a higher risk of developing the disease. While the exact cause of prostate cancer is still unknown, certain risk factors such as age, race, family history, and genetics have been associated with an increased likelihood of developing the condition.
One of the challenges of prostate cancer is that it often does not cause noticeable symptoms in the early stages. This means that many men may have the disease without knowing it, making regular screenings and early detection crucial for successful treatment. Some symptoms that may occur as prostate cancer progresses include difficulty urinating, blood in the urine or semen, erectile dysfunction, and bone pain.
Diagnosing prostate cancer usually involves a combination of physical exams, blood tests, imaging tests, and biopsies. The prostate-specific antigen (PSA) test is a common tool used to screen for prostate cancer, although it is not foolproof and may lead to false-positive results. If a suspicious lump or abnormality is found during a physical exam or imaging test, a biopsy may be performed to confirm the presence of cancerous cells.
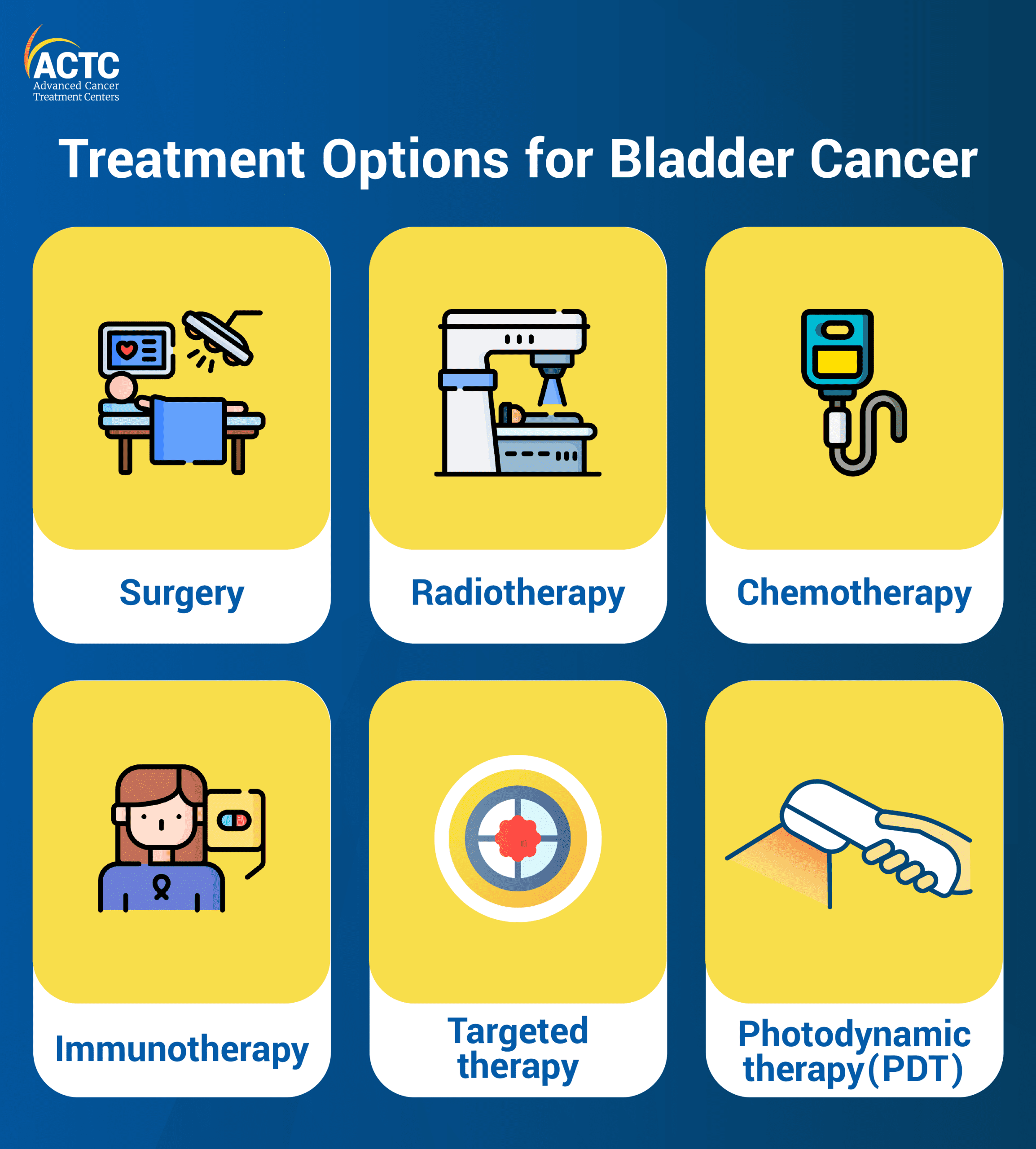
Once prostate cancer is diagnosed, the treatment options will depend on various factors, including the stage of the cancer, the patient’s age and overall health, and personal preferences. Treatment options for prostate cancer may include active surveillance, surgery, radiation therapy, hormone therapy, chemotherapy, and immunotherapy. The goal of treatment is usually to remove or destroy the cancerous cells and prevent the cancer from spreading to other parts of the body.
It is important for men to be aware of the risk factors for prostate cancer and to speak with their healthcare providers about screening options. While not all cases of prostate cancer require immediate treatment, early detection and intervention can greatly improve the chances of successful outcomes. By understanding the basics of prostate cancer, men can take proactive steps to protect their health and well-being.
Risk Factors for Prostate Cancer Mortality
Prostate cancer is a common form of cancer among men, and it is essential to understand the risk factors that can contribute to mortality from the disease. While age is a significant risk factor for prostate cancer development, several other factors can also increase the likelihood of mortality among patients. Here are some of the key risk factors for prostate cancer mortality:
1. Advanced Stage at Diagnosis: One of the most critical risk factors for prostate cancer mortality is the stage at which the disease is diagnosed. Patients who are diagnosed with advanced-stage prostate cancer typically have a poorer prognosis and are more likely to succumb to the disease. This underscores the importance of early detection through regular screenings such as prostate-specific antigen (PSA) tests and digital rectal exams.
2. High Gleason Score: A high Gleason score is another significant risk factor for prostate cancer mortality. The Gleason score is a grading system that measures the aggressiveness of prostate cancer cells based on their appearance under a microscope. Patients with a high Gleason score are more likely to have fast-growing, aggressive tumors that are harder to treat effectively. These patients often require more aggressive treatment options, such as surgery, radiation therapy, or chemotherapy, to improve their chances of survival.
3. Metastasis: Prostate cancer that has spread beyond the prostate gland to other parts of the body, also known as metastatic prostate cancer, is associated with a higher risk of mortality. Once prostate cancer metastasizes, it becomes much more challenging to treat and control, leading to a poorer prognosis for patients. Metastatic prostate cancer may require more intensive treatment modalities, such as hormone therapy, immunotherapy, or targeted therapy, to manage the spread of the disease and prolong survival.
4. Ethnicity: Studies have shown that ethnicity can also play a role in prostate cancer mortality rates. African American men have been found to have a higher incidence of prostate cancer and are more likely to die from the disease compared to men of other racial or ethnic backgrounds. This disparity may be attributed to various factors, including genetic predisposition, access to healthcare, and socioeconomic disparities. It is essential for healthcare providers to consider ethnicity as a risk factor when assessing prostate cancer mortality risk in patients.
5. Comorbidities: Medical conditions such as diabetes, heart disease, obesity, and hypertension can also impact the prognosis of prostate cancer patients. Patients with pre-existing comorbidities may be at a higher risk of mortality due to the challenges posed by managing multiple health conditions simultaneously. It is crucial for healthcare providers to address and manage comorbidities effectively to improve the overall prognosis and quality of life for prostate cancer patients.
By understanding and addressing these risk factors for prostate cancer mortality, healthcare providers can better tailor treatment plans and interventions to improve outcomes for patients diagnosed with the disease. Early detection, timely intervention, and a comprehensive approach to care are key components in reducing mortality rates and improving the overall survival of prostate cancer patients.
Screening and early detection for Prostate Cancer
Prostate cancer is one of the most common types of cancer in men, with a high mortality rate if not detected early. Screening plays a crucial role in detecting prostate cancer at an early stage, when it is more treatable. Screening tests for prostate cancer include the prostate-specific antigen (PSA) test and digital rectal exam.
The PSA test measures the level of PSA in the blood, which is a protein produced by the prostate gland. Elevated PSA levels may indicate the presence of prostate cancer, although other factors such as age and prostate size can also affect PSA levels. The digital rectal exam involves a healthcare provider inserting a gloved, lubricated finger into the rectum to feel for any abnormalities in the prostate gland.
It is recommended that men discuss the benefits and risks of prostate cancer screening with their healthcare provider, as screening may lead to false-positive results and unnecessary biopsies. In some cases, slow-growing prostate cancers may be monitored through active surveillance rather than immediately treated.
Men with a family history of prostate cancer or certain genetic mutations may be at a higher risk for developing the disease, and should speak with their healthcare provider about the appropriate screening schedule for early detection. African American men are also at a higher risk for prostate cancer and may benefit from earlier and more frequent screening.
Early detection of prostate cancer through screening can significantly increase the chances of successful treatment and survival. It is important for men to be proactive about their health and discuss screening options with their healthcare provider. By staying informed and aware of the risks and benefits, men can take control of their prostate health and potentially prevent the progression of prostate cancer to a more advanced and less treatable stage.
Treatment options for Advanced Prostate Cancer
When prostate cancer has progressed to an advanced stage, treatment options may become more limited. However, there are still several approaches that can help manage the disease and alleviate symptoms. Here are some common treatment options for advanced prostate cancer:
Hormone Therapy: Hormone therapy, also known as androgen deprivation therapy, is a common treatment for advanced prostate cancer. This type of therapy works by reducing the levels of male hormones (androgens) in the body, which can help slow the growth of prostate cancer cells. Hormone therapy may involve taking medications that block the production of androgens, such as leuprolide or flutamide, or surgically removing the testicles, which are a major source of androgens. Although hormone therapy can be effective in controlling the progression of prostate cancer, it may have side effects such as hot flashes, fatigue, and loss of libido.
Chemotherapy: Chemotherapy is another treatment option for advanced prostate cancer. This type of treatment uses drugs to kill cancer cells or prevent them from dividing. Chemotherapy is often used when hormone therapy is no longer effective or when the cancer has spread to other parts of the body. Common chemotherapy drugs for prostate cancer include docetaxel, cabazitaxel, and mitoxantrone. While chemotherapy can be effective in slowing the progression of the disease, it can also cause side effects such as nausea, hair loss, and fatigue.
Radiation Therapy: Radiation therapy uses high-energy beams to target and kill cancer cells. This treatment can be used to shrink tumors, alleviate pain, or slow the spread of the disease. In some cases, radiation therapy may be used in combination with hormone therapy or chemotherapy. There are several types of radiation therapy for prostate cancer, including external beam radiation therapy, brachytherapy, and stereotactic body radiation therapy. Side effects of radiation therapy may include fatigue, skin irritation, and urinary problems.
Immunotherapy: Immunotherapy is a relatively new treatment approach for advanced prostate cancer. This type of therapy works by boosting the body’s immune system to help it recognize and attack cancer cells. Immunotherapy drugs such as sipuleucel-T and pembrolizumab have been approved for the treatment of advanced prostate cancer. While immunotherapy can be effective in some patients, it may also cause side effects such as fatigue, rash, and flu-like symptoms.
In addition to these treatments, there are also clinical trials and experimental therapies available for advanced prostate cancer. These may include targeted therapies, gene therapy, or combination treatments. It’s important for patients with advanced prostate cancer to work closely with their healthcare team to explore all available treatment options and create a personalized treatment plan that meets their needs and goals.
Supportive Care for Patients with Prostate Cancer
Supportive care for patients with prostate cancer is essential in helping them cope with the physical, emotional, and psychological challenges that come with the disease. Prostate cancer can have a significant impact on a patient’s quality of life, as well as their ability to carry out daily activities. Therefore, it is important for healthcare providers to offer comprehensive supportive care to address these needs.
1. Pain Management:
Pain is a common symptom of advanced prostate cancer, and effective pain management is crucial in improving the patient’s quality of life. This may involve the use of pain medications, physical therapy, or alternative therapies such as acupuncture or massage. It is important for healthcare providers to work closely with the patient to develop a personalized pain management plan that addresses their individual needs and preferences.
2. Emotional Support:
Receiving a diagnosis of prostate cancer can be a challenging and emotional experience for patients. It is essential for healthcare providers to offer emotional support to help patients cope with their feelings of fear, anxiety, and uncertainty. This may involve counseling, support groups, or connecting the patient with a mental health professional. Providing a safe space for patients to express their emotions and fears can be incredibly beneficial in helping them navigate their cancer journey.
3. Nutritional Support:
Nutrition plays a crucial role in the overall health and well-being of patients with prostate cancer. Treatment for prostate cancer, such as surgery, radiation therapy, or hormonal therapy, can have a significant impact on the patient’s appetite and nutritional needs. Healthcare providers should work with patients to develop a personalized nutrition plan that ensures they are getting the necessary nutrients to support their treatment and recovery. This may involve working with a registered dietitian to address any specific dietary concerns or restrictions.
4. Exercise Programs:
Regular physical activity can have numerous benefits for patients with prostate cancer, including improving physical strength, reducing fatigue, and enhancing overall quality of life. Healthcare providers should encourage patients to engage in regular exercise programs that are tailored to their individual abilities and preferences. This may involve activities such as walking, swimming, yoga, or strength training. By staying active, patients can improve their physical and emotional well-being throughout their cancer journey.
5. Financial Support:
Dealing with a cancer diagnosis can be expensive, and financial concerns can add additional stress to an already challenging situation. Healthcare providers should be proactive in connecting patients with resources and support services that can help alleviate financial burdens. This may include assistance with insurance claims, accessing financial aid programs, or connecting patients with social workers who can provide guidance on managing medical expenses. By addressing financial concerns proactively, healthcare providers can help patients focus on their treatment and recovery without the added stress of financial worries.
Originally posted 2025-05-12 23:31:55.